Knee replacement procedure - Mr Nigel Willis
Introduction
This information, compiled by Nigel Willis, is designed to ensure that you understand what is involved with your upcoming knee replacement surgery and what to expect before, during and after the procedure. Understanding and following these instructions is paramount in order to maximise the benefits of surgery. Mr Willis, physiotherapists and nurses will help further educate you on all matters relating to the procedure.
There are potential complications that may occur during or after knee replacement surgery, however Mr Willis will inform you about these prior to you agreeing to undergo the procedure. Being an elective procedure means that you can choose not to have it performed if you are not willing to accept the risks involved. Rather than undergoing surgery, you may choose to continue with conservative (non-operative) treatment of your condition.
-
What is knee replacement?
What is knee replacement surgery?
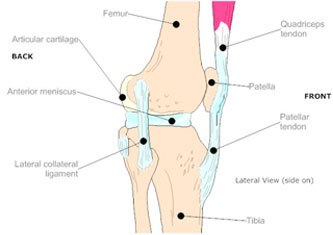
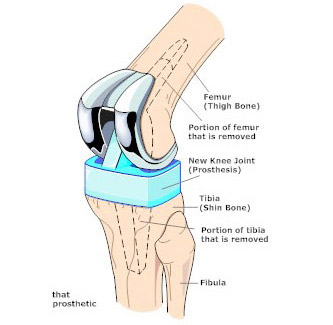
Knee replacement is a surgical procedure where worn, diseased, or damaged surfaces of a knee joint are removed and replaced with artificial surfaces. Materials used for resurfacing of the joint are not only strong and durable but also optimal for joint function as they produce as little friction as possible.
The artificial joint (prosthesis) generally has two components, one made of metal which is usually cobalt -chrome or titanium. The other component is a plastic material called polyethylene.
Why is knee replacement performed?
The most common reason for knee replacement surgery is severe arthritis of the knee that causes pain and stiffness of the knee joint, to the point where it seriously restricts your movement and quality of life. Your doctor is likely to recommend a knee replacement only when other treatments for your arthritis (such as medication, physiotherapy and exercise) are no longer effective.
Less commonly, a knee replacement may also be necessary due to knee damage or decline caused by rheumatoid arthritis, haemophilia, gout, or bone death or bone growth disorders.
The overall goal of knee replacement is designed to provide painless and unlimited standing, sitting, walking, and other normal activities of daily living.
-
What happens prior to surgery?
It is important that you pre-arrange added home assistance, which you are likely to need after you have been discharged from hospital.
You should also arrange transport from the hospital back to your home.
Most patients will be admitted to hospital the day of surgery. Hospital staff will look after your clothes and toiletries whilst you are in surgery. Any valuables should be left with family, a partner or friend.
Nigel Willis will ask you about your general health, medication and any allergies prior to surgery, to ensure that you are fit for the procedure. You can continue to take all of your regular medication, such as pills for high blood pressure, diabetes or heart problems. It is important that you immediately report any infections, particularly relating to skin, urine and teeth.
You will have the opportunity to ask questions prior to the procedure being performed.
-
The surgical procedure
An artificial knee joint (prosthesis) has smooth surfaces which replace the worn surfaces within the knee joint. The prosthesis is made of metal and hard plastic components that fit together during surgery. The surgeon chooses the most appropriate prosthesis design for each patient.
The procedure begins with an incision being made over the front of the knee joint. The surgeon will expose the knee joint, loosen the muscles and ligaments surrounding it, and turn the kneecap out of its place. The worn surfaces within the joint, including the back part of the kneecap, are removed and the ends of the bones are precisely reshaped. The components of the artificial knee joint are then attached to the bone ends using specialised bone cement, and fitted together. The muscles and ligaments are repositioned and, if necessary, the ligaments are re-adjusted to achieve the best possible knee function.
At the completion of the surgery a tube will be inserted to drain excess fluid from the new joint. The surgeon then closes the layers of tissue and the skin with stitches and a dressing is placed around the knee.
Antibiotics are given during and after the operation to prevent the development of infection in the new joint. A blood transfusion may also be required. This will be discussed by the surgeon prior to surgery.
-
Risks & complications of the procedure
As with any surgical procedure, there are risks involved with knee joint replacement. Fortunately, well over 90% of patients who undergo knee replacement surgery have good results. The main risks include:
Anesthesia
Problems can arise when the anesthesia given during surgery that causes a reaction with other drugs that the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Blood clots
Blood clots in the large veins (deep venous thrombosis, or DVT) of the leg and pelvis are common after orthopaedic surgery, especially joint replacement surgery. The risk of developing a blood clot depends on several factors including the type of surgery, other medical problems, medications you may be taking, smoking history, as well as other factors.
Blood loss
Blood loss is a part of surgery. Some surgeries, such as knee replacement, incur blood loss that can lower your blood count after the procedure. If you develop a post-operative anemia, or low blood count, a transfusion may be recommended.
Infection of the replacement joint
One of the main problems associated with knee joint replacements is that infections of these implanted joints can become a very serious problem. This can occur any time, from the day after surgery to several years later. However you can follow specific steps in order to help prevent the onset of infection. Some of the steps you should take are to:
- • Arrange to see your doctor to treat all suspected urinary tract infections.
- • Look for signs of knee infection, including pain, redness, swelling or increased warmth.
- • Establish the restrictions of all activities prior to undertaking them.
- • Advise your dentist of your knee replacement.
-
What happens after surgery?
Once you return to your hospital room you will be required to rest quietly overnight. You will use the deep breathing machine and be given coughing exercises to help clear your lungs and prevent pneumonia. You will also be given the following:
- • Regular medications you took before the operation.
- • Intravenous antibiotics for the first 24 hours.
- • Pain relief medications (either pills or a pain pump).
- • Blood thinners.
The nursing staff will check your pulse, blood pressure, temperature and your leg at regular intervals.
In most cases you will be able to walk the next day. You will be given a few set bedside exercises by your physician or physical therapist. Specific physical goals will be set by Nigel Willis and your therapist and once these have been met, you will be permitted to return home.
You will be given crutches or a walker for approximately six weeks following surgery. Here are other instructions that you will need to adhere to:
- • Sleep with a pillow between your legs for six weeks.
- • Do NOT drive for six weeks.
- • Avoid domestic air travel for six weeks and international air travel for three months.
- • You may walk unlimited distances.
- • Avoid sitting for long periods with your legs down, as this will cause swelling.
- • Return to the office for suture removal two weeks after surgery.
We advise that you contact the rooms or the hospital if you have any concerns or problems, such as bleeding, persistent oozing from the wound, unexplained swelling, increasing pain or general illness. These should be investigated, rather than ignored.
Please advise Nigel Willis or your nurse of any medical conditions that you may have.
-
Rehabilitation
Following surgery, your surgeon and a physiotherapist will work together to set recovery and movement guidelines. Initially these include passive exercises, before progressing to gentle knee bending exercises and walking. Ongoing exercises are designed to increase the range of motion of the new joint and to strengthen the surrounding muscles, particularly the thigh muscle (quadricep). Strength in the quadricep will help to keep the knee joint stable, therefore protecting the new joint.
The success of the surgery depends on following the recovery and movement instructions while in hospital and on carrying out the prescribed exercises when at home.
Once you are back at home, you will be required to perform a number of exercises twice a day. They are as follows:
Gluteal sets
While lying on your back, tighten your buttock muscles. Hold tightly for 5 seconds. Repeat 10 times.
Quadriceps sets
This is an isometric exercise, where there is no movement involved. Tighten the quadriceps muscles by pressing the back of your knee flat, tightening the kneecap (patella). Look for visible contraction, especially on the inside of the thigh by the knee. Hold for 5 seconds, then release. Repeat 10 times.
Ankle pumping
Increase range of motion and circulation by first pointing your toes downward, then up in a slow steady motion. Repeat 10 times.
Heal to buttock, long sitting
Bend your affected knee approximately 45 degrees as you slide your heel towards your buttock. As tension develops, hold for 5 seconds and then slide heel to the starting position. Do 10 repetitions.
Terminal knee extension, supine
Lie on your back with a towel roll under your knee. Straighten your knee (still supported by the roll) and hold for 5 seconds. Slowly return to the starting position. Repeat 10 times. For an advanced form of this exercise, add 5 pounds at the ankle before beginning.
Please note that this orthopaedic surgery procedure is elective (you can choose to have this surgery or not). The decision to choose surgery is made at the end of a thorough consultative process between you, your othopaedic surgeon and where required, other medical specialists.
It is very rare where two people have exactly the same issue, so each procedure and post-surgery treatment is specifically diagnosed and tailored to your individual requirements.
Therefore, the information provided here is for general advice only and is not a substitute for a consultation appointment with your orthopaedic surgeon.
For consultations with Mr Nigel Willis, please ask your GP for a referral.