ACL Reconstruction procedure - Mr Nigel Willis
Introduction
This information, compiled by Nigel Willis, is designed to ensure that you understand what is involved with your upcoming ACL reconstruction surgery and what to expect before, during and after the procedure. Understanding and following these instructions is paramount in order to maximise the benefits of surgery. Mr Willis, physiotherapists and nurses will help further educate you on all matters relating to the procedure.
There are potential complications that may occur during or after ACL reconstruction surgery, however Mr Willis will inform you about these prior to you agreeing to undergo the procedure. Being an elective procedure means that you can choose not to have it performed if you are not willing to accept the risks involved. Rather than undergoing surgery, you may choose to continue with conservative (non-operative) treatment of your condition.
-
What is ACL reconstruction?
ACL reconstruction surgery
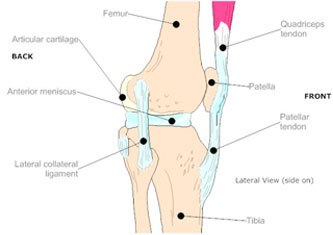
ACL reconstruction surgery involves replacing the ligament in the centre of your knee with a new ligament. The anterior cruciate ligament (ACL) keeps your shin bone (tibia) in place. A tear of this ligament can cause your knee to give way during physical activity.
ACL tears are not usually repaired using suture to sew it back together because repaired ACLs have generally been shown to fail over time. Therefore, the torn ACL is generally replaced by a substitute graft made of tendon. The grafts commonly used to replace the ACL include:- • Patellar tendon autograft (autograft comes from the patient)
- • Hamstring tendon autograft
- • Quadriceps tendon autograft
- • Allograft (taken from a cadaver) patellar tendon, Achilles tendon, semitendinosus, gracilis, or posterior tibialis tendon
The goal of the ACL reconstruction surgery is to prevent instability and restore the function of the torn ligament, creating a stable knee. This allows the patient to return to sports. There are certain factors that the patient must consider when deciding for or against ACL surgery.
Why the procedure is performed
One of the most common knee injuries is an ACL sprain or tear. We know that not treating a torn ACL can lead to tissue damage and early arthritis. ACL reconstruction may be recommended for these knee problems:
- • Knee that gives way or feels unstable during daily activities
- • Knee pain
- • Inability to continue playing sports or other activities, especially ones with cutting or pivoting
- • Other ligaments are also injured
-
What happens prior to surgery?
Before surgery, Nigel Willis will ask you about your general health, medication and any allergies prior to surgery, to ensure that you are fit for the procedure. You can continue to take all of your regular medication, such as pills for high blood pressure, diabetes or heart problems.
If you take Asprin, you must stop taking it one week prior to surgery.
It is important that you immediately report any infections, particularly relating to skin, urine and teeth.
Most patients will be admitted to hospital the day of surgery. Hospital staff will look after your clothes and toiletries whilst you are in surgery. Any valuables should be left with family, a partner or friend.
It is important that you pre-arrange added home assistance before the procedure is performed.
You should also arrange transport from the hospital back to your home. You will have the opportunity to ask questions prior to the procedure being performed.
-
The surgical procedure
The majority of surgeons perform this surgery using an arthroscope, a small fiber-optic TV camera that is used to see and operate inside the joint. Only small incisions are needed during arthroscopy for this procedure. The operation doesn't require the surgeon to open the knee joint.
Before surgery you will be placed under either general anesthesia, or a type of spinal anesthesia. The surgeon begins the operation by making two small incisions in the knee, called portals. These portals are where the arthroscope and surgical tools are placed into the knee. Care is taken to protect the nearby nerves and blood vessels.
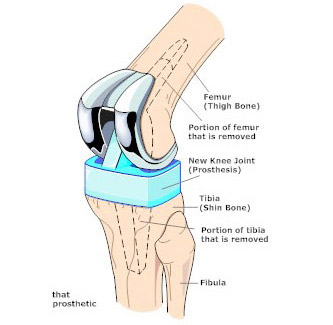
A small incision is also made below the patella. Working through this incision, the surgeon takes out the middle section of the patellar tendon, along with the bone attachments on each end. The bone plugs are rounded and smoothed. Holes are drilled in each bone plug to place sutures (strong stitches) that will pull the graft into place.
Next, the surgeon prepares the knee to place the graft. The remnants of the original ligament are removed. The intercondylar notch (the deep fossa between the femoral condyles in which the cruciate ligaments are attached) is enlarged so that nothing will rub on the graft. This part of the surgery is referred to as a notchplasty.
Once this is done, holes are drilled in the tibia and the femur to place the graft. These holes are placed so that the graft will run between the tibia and femur in the same direction as the original ACL.
The graft is then pulled into position using sutures placed through the drill holes. Screws are used to hold the bone plugs in the drill holes.
To keep fluid from building up in your knee, the surgeon may place a tube in your knee joint. The portals and skin incision are then stitched together, completing the surgery.
-
Risks & complications of the procedure
Some of the most common complications following patellar tendon graft reconstruction of the ACL are:
Anesthesia
Problems can arise when the anesthesia given during surgery that causes a reaction with other drugs that the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Blood clots
Blood clots in the large veins (deep venous thrombosis, or DVT) of the leg and pelvis are common after orthopaedic surgery, especially reconstructive surgery. The risk of developing a blood clot depends on several factors including the type of surgery, other medical problems, medications you may be taking, smoking history, as well as other factors.
Blood loss
Blood loss is a part of surgery. Some surgeries, such as ACL reconstruction, incur blood loss that can lower your blood count after the procedure. If you develop a post-operative anemia, or low blood count, a transfusion may be recommended.
Infection
The chance of getting an infection following ACL reconstruction is very low. Yet precautions are taken before and after the procedure to prevent this serious complication. Antibiotics are given intravenously just before the start of surgery and again after surgery. Proper care of the surgical incisions by the nursing staff, and thorough education about proper incision care prior to discharge from the surgical center, will limit the chance of infection. The meticulous work of the surgeon is another important factor in preventing infection.
Graft Impingement
If the drill holes in the bone (the bone tunnels that were made to hold the new ACL) are incorrectly placed, then the newly placed graft may press against the bone as the knee bends or straightens, and restrict the normal movement of the knee. Most commonly, it becomes impossible to fully straighten the knee. Occasionally this problem may resolve with physical therapy. Usually, another arthroscopic procedure is required to shave away some of the obstructing bone to give more room for the new graft. This may not resolve the problem and further surgery may be required to drill new tunnels in order to place the graft in the proper position inside the knee.
Problems at the Donor Site
Problems can occur at the donor site (the area below the patella where the graft was taken from the knee). A major drawback of taking out a piece of the patellar tendon to reconstruct the ACL is that most patients end up having difficulty kneeling down long after surgery. Lingering pain in the front of the knee is also common.
A portion of bone is taken from the bottom of the patella during the graft procedure. This can weaken the patella. In rare cases, heavy use of the quadriceps muscle (on the front of the thigh) can cause the patella to fracture. This often requires a second surgery to repair the broken patella. Taking tissue from the centre of the patellar tendon can also cause problems. The body attempts to heal the area but sometimes produces too much scar tissue. The extra scar tissue that forms around the donor site may prevent normal motion in the knee. The patellar tendon is not as strong as it was before surgery. In rare cases, this has been linked to a tear in the patellar tendon. Also, the patellar tendon may become easily inflamed. And problems in this area can keep the quadriceps from regaining normal control and strength.
-
What happens after surgery?
Patients generally stay in the recovery room following surgery. Depending on the type of anesthetic that was used, it takes about one to two hours to recover enough to be able to sit up, eat some light food, use the bathroom (with crutches), and feel ready to go home.
Some surgeons prefer their patients remain in the hospital overnight. Other surgeons are happy for their patients to return home four to six hours after surgery.
The nursing staff will educate patients about home medications and will give instructions about when to change the surgical dressing.
You will be given the following:
- • Regular medications you took before the operation.
- • Intravenous antibiotics for the first 24 hours.
- • Pain relief medications (either pills or a pain pump)
- • Blood thinners.
Even though many ACL surgeries are now done as outpatient procedures, the individual will not be able to drive home from the hospital.
- • Before you leave for home, education will be given by the nursing staff regarding pain control as well as care of the incisions.
- • Crutch training (how to use crutches) will be done at that time or may have already been done before the surgery.
- • Depending on the preference of the surgeon, weight bearing will usually be allowed.
- • Crutches are usually needed for at least a week or two, with gradual progression to one crutch and finally to independent walking.
- • Also depending on the surgeon's preference, a brace may or may not be used. Some surgeons prescribe a rehabilitation brace that is adjustable and can be locked in a straight position or set to allow a certain amount of movement. Sometimes, a brace that prevents all bending movements may be used. However in either case, the brace will normally be taken off for certain exercises.
-
Rehabilitation
About a week after the surgery, the physician will inspect the knee and discuss a rehab program. This will be done on an outpatient basis and may begin one to two weeks after surgery. The rehabilitation is very important and has a significant impact on the outcome of the knee and your ability to perform everyday tasks.
The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. The goal is to help you regain full knee extension as soon as possible.
The physical therapist will choose treatments to get the quadriceps muscles toned and active again. Muscle stimulation and biofeedback, which involve placing electrodes over the quadriceps muscle, may be needed at first to get the muscle going again and to help retrain it.
As the rehabilitation program evolves, more challenging exercises are chosen to safely advance the knee's strength and function. Specialized balance exercises are used to help the muscles respond quickly and without thinking. This part of treatment is called neuromuscular training. If you need to stop suddenly, your muscles must react with just the right amount of speed, control, and direction. After ACL surgery, this ability doesn't come back completely without exercise.
Neuromuscular training includes exercises to improve balance, joint control, muscle strength and power, and agility. Agility makes it possible to change directions quickly, go faster or slower, and improve starting and stopping. These are important skills for walking, running, and jumping, and especially for sports performance.
When you get full knee movement, your knee isn't swelling, and your strength and muscle control are improving, you'll be able to gradually go back to your work and sport activities. Some surgeons prescribe a functional brace for athletes who intend to return quickly to their sports.
Ideally, you'll be able to resume your previous lifestyle activities. However, athletes are usually advised to wait at least six months before returning to their sports. Most patients are encouraged to modify their activity choices.
You will probably be involved in a progressive rehabilitation program for four to six months after surgery to ensure the best result from your ACL reconstruction. In the first six weeks following surgery, expect to see the physical therapist two to three times a week. If your surgery and rehabilitation go as planned, you may only need to do a home program and see your therapist every few weeks over the four to six month period.
Please note that this orthopaedic surgery procedure is elective (you can choose to have this surgery or not). The decision to choose surgery is made at the end of a thorough consultative process between you, your othopaedic surgeon and where required, other medical specialists.
It is very rare where two people have exactly the same issue, so each procedure and post-surgery treatment is specifically diagnosed and tailored to your individual requirements.
Therefore, the information provided here is for general advice only and is not a substitute for a consultation appointment with your orthopaedic surgeon.
For consultations with Mr Nigel Willis, please ask your GP for a referral.